Pulmonary Embolism: A Fatal Reality
- Siphosami Ndala
- Jul 5, 2025
- 5 min read
What is Pulmonary Embolism?
Pulmonary embolism (PE) is a condition in which a blood clot or clots cause a life-threatening blockage in the arteries found in the lungs. What makes pulmonary embolism so dangerous is how quickly the symptoms can escalate in severe cases, leading to a critical state, and even death if not promptly managed. The fatality of pulmonary embolism depends on the size of the blood clot that clogs the arteries in the lungs, or when more than one blood clot moves up to the bilateral arteries on both the lungs, completely cutting off oxygen supply. With little understanding of the etiology of pulmonary embolism, many sudden deaths attributed to PE have left millions of family members seeking answers for the untimely loss of their loved ones.

What are the risk factors of Pulmonary Embolism
There are several risk factors that place patients at higher risks to having an episode of an acute pulmonary embolism. Some risks are considered genetic, while others are lifestyle-imposed. Some, however, can be due to predisposed previous or current medical conditions that patients have. The more risk factors a patient has, the more likely a patient is to suffer from pulmonary embolism.
Deep Vein Thrombosis (DVT): One of the most commonly known causes of pulmonary embolism is deep vein thrombosis (DVT). This occurs when a blood clot that formed in a deep vein of the lower limbs travels through the blood stream to the lung blood vessels and clogs them, causing a pulmonary embolism.
Genetic blood-related conditions: There are a few inherited blood-clotting disorders that increase the likelihood of pulmonary embolism. These conditions are called inherited thrombophilia disorders with a characteristic of increased clotting formation, also known as hypercoagulability. Patients with these conditions inherit them from birth and thus are difficult to diagnose unless early investigations are made, based on known family medical history or an incident like an injury occurs leading to its discovery.
Medical conditions: Some chronic conditions like renal failure, heart failure and cancer affect some blood production processes of platelet cells, compromising the clotting capacity in a patient. These conditions are further aggravated or rather the risk increased by their line of treatment protocols, as in the use of chemotherapy and radiotherapy in cancer, and the use of hemodialysis in chronic renal failure. In recent years, it has been discovered that COVID-19 is another huge risk factor that places patients at a higher risk of suffering from pulmonary embolism as COVID-19 affects a patient’s hypercoagulable state.
Major Surgery: Another potentially high-risk factor for pulmonary embolism is major surgery. Patients who are booked for major surgical procedures are prophylactically given anticoagulants pre- and post-surgery in order to mitigate the risk of pulmonary embolism. These medicines work by thinning out blood as a way of preventing the formation of blood clots in the vessels. The reason why major surgeries create a higher risk for PE is because a big operation interferes with multiple vascular connections, increasing the risk of hypercoagulation. Additionally, major surgeries lead to long periods of inactivity due to longer recuperation time. Immobility is considered a risk factor for pulmonary embolism. Surgeries like total abdominal hysterectomies, joint replacements and heart bypass surgeries, are examples of high-risk operations for such venous thromboembolism (VTE) conditions like PE.
Pregnancy: One obvious PE risk factor is pregnancy. It is because pregnancy creates abdominal pressure as the baby grows in the uterus, restricting blood flow in the lower part of the body thus slowing down circulation which creates an opportunity for blood-clot creation. Due to hormonal changes in pregnancy during the three different phases of it- antepartum, peripartum and postpartum, there is a notable and significant decrease in blood thinning activity (anticoagulation) as well as blood clotting processes (fibrinolysis). Both these lay the foundation for venous thromboembolism complications.
Lifestyle-Related Conditions: Other risk factors that increase the probability of a pulmonary embolus are lifestyle related. These include heavy smoking, morbid obesity, and the use of contraceptive pills or hormone replacement therapy (HRT) treatment. Prolonged periods of immobility may also pose a risk for pulmonary embolism. Cases such as inactivity during long-drive trips or lengthy flights, over 8 hours with limited movement, increase VTE risk. Patients over the age of 60 are also at a higher risk of getting PE compared to younger people.
Signs and Symptoms of Pulmonary Embolism
Depending on the severity of the embolism in the lung/s, signs and symptoms may vary in degrees. A minor PE could present as a minor tightness of the chest and may often resolve its own, whereas a massive PE can quickly escalate to sudden cardiac arrest within a few minutes.
Common PE symptoms are:
· A sharp chest pain
· Progressive shortness of breath (dyspnea)
· A feeling of dizziness or even fainting
· A rapid heartbeat (tachycardia)
· Excessive sweating
· Persistent coughing or coughing up blood (hemoptysis)
· Low blood pressure (hypotension)
· Sharp leg pain
· Sudden cardiac arrest
Diagnosing Pulmonary Embolism
CT scan: also known as a Computerized Tomography scan, a chest CT scan is the most reliable diagnostic test for a PE as it gives a much clearer and more detailed picture of the embolism in the lung. It also provides other alternative causes of respiratory distress where PE needs to be excluded. A CT scan can provide precise location of the PE and its size. However, to diagnose PE with a CT scan, contrast dye must be used, which is contraindicated in patients with kidney problems as it could worsen the condition.
VQ scan: also known as a lung Ventilation/Perfusion scan or Isotope scan. VQ scans are the very next best choice after a CT scan to try and diagnose PE. They are often used in patients in whom a CT scan is contraindicated (ie. patients with kidney problems or patients allergic to contrast). A VQ scan is performed by instilling dye into the pulmonary arteries to assess the flow and locate where the blockage is.
D-dimer test: this is a blood test that is used to measure the clotting factor degree in the patient’s blood. Elevated levels of D-dimer are a sign that a blood clot may be present and thus a call for prompt treatment.
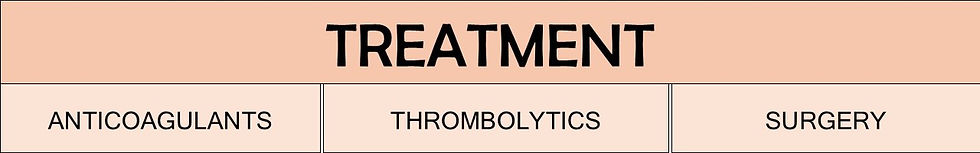
Treatment for Pulmonary Embolism
Anticoagulants: this treatment is also known as blood thinners. They help prevent the formation of blood clots by thinning out the blood.
Thrombolytics: these medications target blood clots and break them down to prevent them from getting bigger and causing blockages in the veins.
Surgery: surgical interventions like an embolectomy or thrombectomy can be done in cases where all other treatments have failed. Surgery is more invasive. An incision is made where the clot is and can either be suctioned out via a catheter or removed directly via a median sternotomy (chest cavity incision) which is a major procedure.
Though pulmonary embolism can be fatal, it is crucial for any patient with presenting symptoms to seek urgent medical help. With prompt treatment, any patient can survive and recover from a pulmonary embolism.
REFERENCES
Hudson, R. (2023) Pulmonary embolism. Available at: https://patient.info/signs-symptoms/breathlessness-and-breathing-difficulties-dyspnoea/pulmonary-embolism (Accessed on: 28/05/2025)
Ouellette, D. (2024) Pulmonary Embolism (PE). Available at: https://emedicine.medscape.com/article/300901-overview (Accessed on: 28/05/2025)
Bull, TM., Hountras, P. (2025) Pulmonary Embolism (PE). Available at: https://www.msdmanuals.com/professional/pulmonary-disorders/pulmonary-embolism/pulmonary-embolism-pe (Accessed on: 28/05/2025)
Krans, B. (2021) Pulmonary Embolism (Blood Clot in the Lung): Symptoms and More. Available at: https://www.healthline.com/health/pulmonary-embolus (Accessed on: 28/05/2025)
Curtis, L. (2023). What is Pulmonary Embolism? Available at: https://www.health.com/pulmonary-embolism-overview-7109333 (Accessed on: 30/05/2025)
Gersten, T. (2023) Pulmonary embolus. Available at: https://medlineplus.gov/ency/article/000132.htm (Accessed on: 30/05/2025)
Lo, DS., Rabbat, CG., Clase, CM. (2005) Thromboembolism and anticoagulant management in hemodialysis patients: A practical guide to clinical management. Available at: https://www.sciencedirect.com/science/article/abs/pii/S0049384805002148 (Accessed on: 05/06/2025)
Biedka, M., Ziolkowska, E., Windorbska, W. (2012) Acute pulmonary embolus in the course of cancer. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC3687454/#S0002 (Accessed on: 05/06/2025)
Mayo Clinic Staff. (2022) Pulmonary embolism. Available at: https://www.mayoclinic.org/diseases-conditions/pulmonary-embolism/symptoms-causes/syc-20354647 (Accessed on: 05/06/2025)
Dado, CD., Levinson, AT., Bourjeily, G. (2018) Pregnancy and Pulmonary Embolism. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC8018832/ (Accessed on: 06/06/2025)
Embolectomy. (2022) Available at: https://my.clevelandclinic.org/health/treatments/23340-embolectomy (Accessed on: 20/06/2025)
Assessed and Endorsed by the MedReport Medical Review Board





