Bladder Cancer 101: Symptoms,Causes, and Treatment Options
- Sherry Ainsworth

- Nov 16, 2025
- 7 min read

By Sherry Ainsworth, MSN, RN, ARNP
You wake up one morning and hit the bathroom as usual. Only, this morning there is something different. You notice that your urine is a light shade of brown, or maybe pink. What on earth could that be? If you’ve ever had a bladder infection before, you might think this is a symptom of another one starting up. However, it could be an early warning of bladder cancer. Cancer is sometimes called carcinoma.
What is Bladder Cancer?
Due to reasons not entirely known, some cells in bladder tissue can develop changes in their DNA. DNA’s function is to instruct cells on what to do, and these changes cause the cells to multiply rapidly and form tumors, which are clumps of abnormal cells. The tumors can then destroy normal tissue. Over time, the abnormal cells can separate from the tumors and spread (metastasize) through the body.
How Common Is It?
It is estimated that there will be about 84,870 new cases of bladder cancer in the U.S. in 2025. Of these 65,080 will be male and 4,780 female (American Cancer Society, 2025).
Also, more women than men die of bladder cancer, possibly because women are more likely to overlook their symptoms and report them too late. We will see why in the next section.
What Are the Symptoms?
Blood in the urine (hematuria) is the most common symptom. It is rarely bright red, usually brown or pink. It may not be seen at all, but it may be visible under a microscope. Other symptoms could be having to go more often in small amounts, painful urination, or urination a lot at night (nocturia). Occasionally, bladder or lower abdominal pain can be a symptom. Unfortunately, all these symptoms can easily be mistaken for a UTI (urinary tract infection) or a bladder infection. Women who have had UTIs or bladder infections are more likely to report these symptoms late. Also, women of childbearing age can mistake blood in the urine for menstrual blood.
Who Is at Risk for Bladder Cancer?
Smokers have about three to four times more risk of developing bladder cancer than non-smokers. Smoking is estimated to cause about 50% of all bladder cancers. The American Cancer Society states that smoking is the most critical risk factor for bladder cancer. Smoking e-cigarettes (vaping) can also cause cellular changes in the bladder, developing into cancer cells. Smoking, including e-cigarettes, is known as a “modifiable risk factor” because it is a behavior that can be changed.
Other risk factors include exposure to cancer-causing chemicals, such as dyes or dry-cleaning chemicals like perchloroethylene and trichloroethylene (Callahan, 2019). In addition, metal workers, mechanics, and hairdressers also risk exposure to similar chemicals. Those who work with leather, rubber, textiles, or paints also risk exposure to cancer-causing chemicals. Additionally, men are three times more likely than women to develop bladder cancer, and 90% of all cases happen to those over age 55. Race is also a risk factor: those who are white have twice the risk of African-Americans (McMillen, 2024). Additional risk factors include genetics, previous cancer treatment, chronic bladder irritation, and certain bladder birth defects.
Why is Smoking the Biggest Risk Factor?
Toxins from cigarette smoke not only enter the lungs, they leave the body by way of the urinary tract. The bladder is part of that system, and it is exposed to high concentrations of those toxins while they are held in the urine inside.
Types of Bladder Cancer
· Urothelial (formerly called transitional cell) cancer accounts for 90-95% of all bladder cancer. It develops in the inner layer of the bladder (the urothelial layer).
· Squamous cell cancer – squamous cells are normally found in scattered places in the bladder. They are flat, scaly, and form barriers against bacteria and fluid loss. However, they can become cancerous, especially as a result of chronic irritation.
· Adenocarcinoma starts in gland-forming cells in the bladder.
· Small-cell carcinomas start in neuroendocrine cells in the bladder. They are treated with chemotherapy similar to that used for small-cell lung cancer.
The Spread of Bladder Cancer (Metastasis)
Although urothelial carcinoma is the most common kind, it is important to know how fast this cancer can metastasize into lymph nodes, bones, lungs, or liver. Therefore, it is important to detect it early to start the most effective treatment. “Grade” refers to the degree of abnormality seen when looking at the cells under a microscope. Low-grade cancer usually grows slowly, while high-grade cancer can grow into the muscle wall of the bladder within three months. The most common sites of metastasis are first the pelvic lymph nodes, then the liver and lungs, and then to the bones.
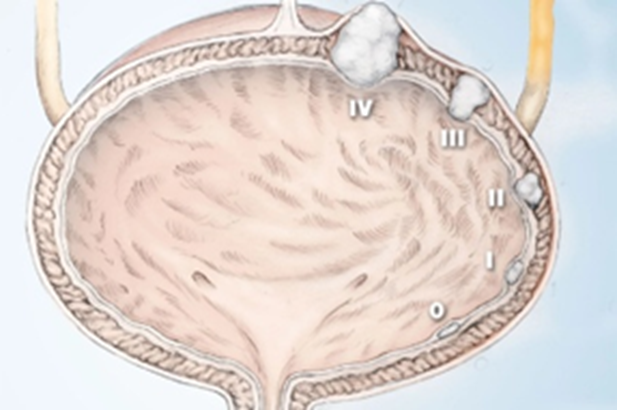
Stages of Bladder Cancer
These stages reflect the extent of growth of a bladder tumor, and in turn affect the survival rate. The lower the stage, the higher the survival rate. All the stages are treatable, and survival depends on the effectiveness of the treatments given, the patient’s tolerance of any side effects, and the patient’s general health.
Stage 0 – Cancer stays in the inner lining,
Stage I – Cancer has spread to the bladder wall,
Stage II - Cancer has grown into the muscle of the bladder wall,
Stage III – Cancer has spread to fatty tissue around the bladder and possibly to nearby lymph nodes. It may also have spread to the prostate in men or the uterus or vagina in women,
Stage IV – Cancer has spread to the pelvic or abdominal wall, and also lymph nodes
(McMilen, 2025).
How Is Bladder Cancer Diagnosed?
· A urinalysis may be done to check for signs of infection and to check for microscopic blood in the urine.
· Blood tests may be done to see if you are losing blood or have signs of infection, or for “tumor markers” (although these are not always specific for cancer).
· If there is no infection but there are signs of blood, you may be referred to a urologist for further tests.
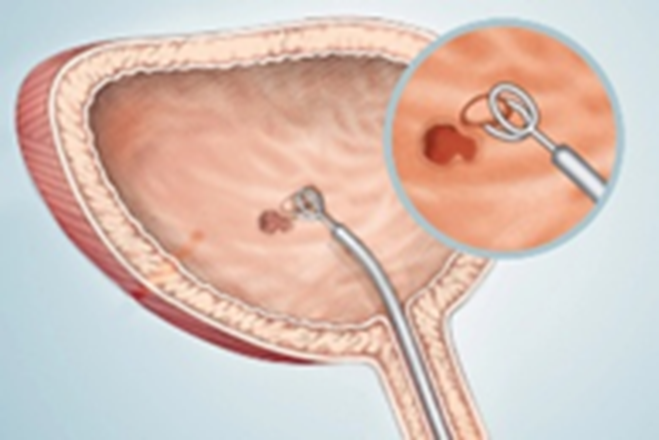
· Cystoscopy – this is a painless procedure usually done in the urology office. The urethra is numbed with sterile lidocaine jelly, and a thin tube called a cystoscope with a tiny light and camera on the end is passed through the urethra into the bladder to inspect the bladder lining. A biopsy can be taken of any tumor found during the cystoscopy, with a tiny wire loop passed through the cystoscope.
· The following is a diagram of what happens during a cystoscopy and biopsy. During the procedure, you will probably be able to watch it on a screen nearby.
· Later tests may include a CT urogram, which is a type of X-ray. Alternatively, the urologist may order an MRI (magnetic resonance imaging) of the bladder, which is not an X-ray, but rather a type of imaging similar to taking a photograph of the bladder.
Treatment Options
For a low-grade, Stage I urothelial cancer, the first treatment is a TURBT (transurethral resection, or removal, of the bladder tumor through the urethra) by the urologist. No external incision is needed, and the procedure is similar to a cystoscopy. It may be done during the diagnostic stage (McMillen 2025).
After the tumor is resected, the urologist may inject one dose of immunotherapy once a week for six weeks. The chemotherapy is usually one called BCG and is injected directly into the bladder via the urethra, to stop any further cancer cells from developing. Or they may use a chemotherapy called Mutamycin. You will need to follow up with the urologist regularly after that for several years, and learn more about the possibility of the return of cancer.
Ongoing Research
Most of the recent research concerning bladder cancer treatments has been focused on targeted therapies, which target proteins that control the growth of the cancer cells.
The FDA now approves several of these treatments. There are also approved antibody drug conjugates, which are now approved for the treatment of advanced or metastatic bladder cancer. There are also combination therapies and gene therapies.
Hope for the Future
Research is ongoing to determine the causes of cancer, and at the same time is exploring effective treatments for bladder cancer and other cancers. Your urologist and your primary care provider will be a great support for you, as well as cancer patient groups you can join for further information and comfort for yourself and your family.

Sherry Ainsworth is a nurse practitioner/freelance writer with over 40 years of experience in nursing. She now writes educational articles and contributes to health-related websites. She lives in Aberdeen, WA, with her husband and two very active cats, and has a 14-year-old granddaughter.
References
Advances in bladder cancer research (October 9, 2024). National Cancer Institute (NIH). https://www.cancer.gov/types/bladder/research
Bladder cancer (2025). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/bladder-cancer/symptoms-causes/syc-20356104?p=1
Bladder cancer: signs & symptoms, diagnosis and treatment (2025). St John’s Cancer Institute. https://www.saintjohnscancer.org/urology/conditions/treatment-for-bladder-cancer/
Callahan, C. L., Stewart, P. A., Blair, A., & Purdue, M. P. (2019). Extended mortality follow-up in a cohort of dry cleaners. Epidemiology (Cambridge, Mass.), 30(2), 285. https://doi.org/10.1097/EDE.0000000000000951
Gilbert, S. (2025). Where does metastatic bladder cancer spread to? Moffitt Cancer Center. https://www.moffitt.org/cancers/bladder-cancer/metastatic-bladder-cancer/where-does-metastatic-bladder-cancer-spread-to/#:~:text=Understanding%20local%20bladder%20cancer%20metastasis,the%20abdominal%20wall%20(peritoneum).
Gontero, P. (2025). Guidelines: Upper urinary tract urothelial cell carcinoma. European Association of Urology (EAU). https://uroweb.org/guidelines/upper-urinary-tract-urothelial-cell-carcinoma/chapter/epidemiology-aetiology-and-pathology
Jones, V. (May 24, 2024). Urothelial carcinoma: 8 insights about this common bladder cancer. MD Anderson Cancer Center. https://www.mdanderson.org/cancerwise/urothelial-carcinoma--8-insights-about-this-common-bladder-cancer.h00-159697545.html
Key Statistics for Bladder Cancer (2025). American Cancer Society.
McMillen, M. (July 9, 2024). Visual guide to bladder cancer. WebMD/Cancer/Bladder/Slideshows. https://www.webmd.com/cancer/bladder-cancer/ss/slideshow-bladder-cancer-overview?ecd=wnl_spr_091225&ctr=wnl-spr-091225_lead_cta&mb=t1C9RUcvibuooue%40W0jX8%40HnVev1imbCoxCAfLcI%40QU%3d
Modglin, L (May 8, 2024). How fast does bladder cancer spread? Patient Power.
The leading cause of bladder cancer: smoking (2025). Bladder Cancer Advocacy Network (BCAN).https://bcan.org/smoking-bladder-cancer-risk/#:~:text=Smoking%20is%20estimated%20to%20contribute,many%20hours%20at%20a%20time.
What is bladder cancer? (March 12, 2024). American Cancer Society.
Assessed and Endorsed by the MedReport Medical Review Board






